Understanding Thoracic Hypomobility: Causes, Effects, and Treatment
Thoracic hypomobility is a condition that significantly affects the mobility and functioning of the thoracic spine, which plays a critical role in overall posture, breathing, and functional movement. Understanding thoracic hypomobility involves exploring its causes, symptoms, implications on health, and effective treatment strategies. In this article, we will delve deep into this commonly overlooked condition to provide comprehensive insights for patients and healthcare professionals alike.
What is Thoracic Hypomobility?
Thoracic hypomobility refers to a decreased range of motion in the thoracic spine, comprising the middle segment of the vertebral column. This decrease in mobility can lead to various complications, including chronic pain, altered posture, and diminished respiratory function. It often stems from a variety of factors, including muscular tightness, poor posture, trauma, or sedentary lifestyle.
Causes of Thoracic Hypomobility
Several factors can contribute to thoracic hypomobility:
- Muscle Imbalances: Tightness in the pectoral muscles can pull the shoulder forward, limiting the movement of the thoracic spine.
- Poor Posture: Prolonged sitting, especially with suboptimal ergonomic setups, can lead to hunching and reduced thoracic mobility.
- Injuries: Trauma to the thoracic spine region, whether from accidents or sports-related injuries, can restrict movement.
- Degenerative Diseases: Conditions like arthritis can lead to stiffness and decreased mobility in the spine.
- Age-related Changes: As we age, the vertebrae and intervertebral discs may lose hydration and elasticity, leading to hypomobility.
Symptoms of Thoracic Hypomobility
Individuals with thoracic hypomobility may experience a range of symptoms, including:
- Chronic Pain: Persistent discomfort in the mid-back region is common.
- Stiffness: Difficulty in twisting, bending, or arching the back can occur, restricting daily activities.
- Reduced Breathing Capacity: The inability to expand the thoracic cavity may lead to shallow breathing and decreased oxygen intake.
- Fatigue: Muscle fatigue can result from compensatory mechanisms due to restricted mobility.
The Impact of Thoracic Hypomobility on Health
Thoracic hypomobility can have far-reaching effects on a person’s health and well-being. The thoracic spine supports vital structures, including the lungs and heart, and any impairment could lead to complications that affect more than just the back.
1. Postural Dysfunctions
Thoracic hypomobility often contributes to postural dysfunctions. A lack of mobility can lead to a condition known as "upper crossed syndrome," where the head protrudes forward and the shoulders round, leading to increased strain on the cervical spine.
2. Respiratory Issues
As the thoracic spine influences rib cage movement, decreased spinal mobility can limit respiratory capacity. This can lead to shallow breathing, which may trigger issues such as anxiety and reduce overall stamina.
3. Increased Risk of Injury
Reduced thoracic mobility can predispose an individual to injuries during activities that require twisting, bending, or lifting, as compensatory movements can place undue stress on other parts of the body.
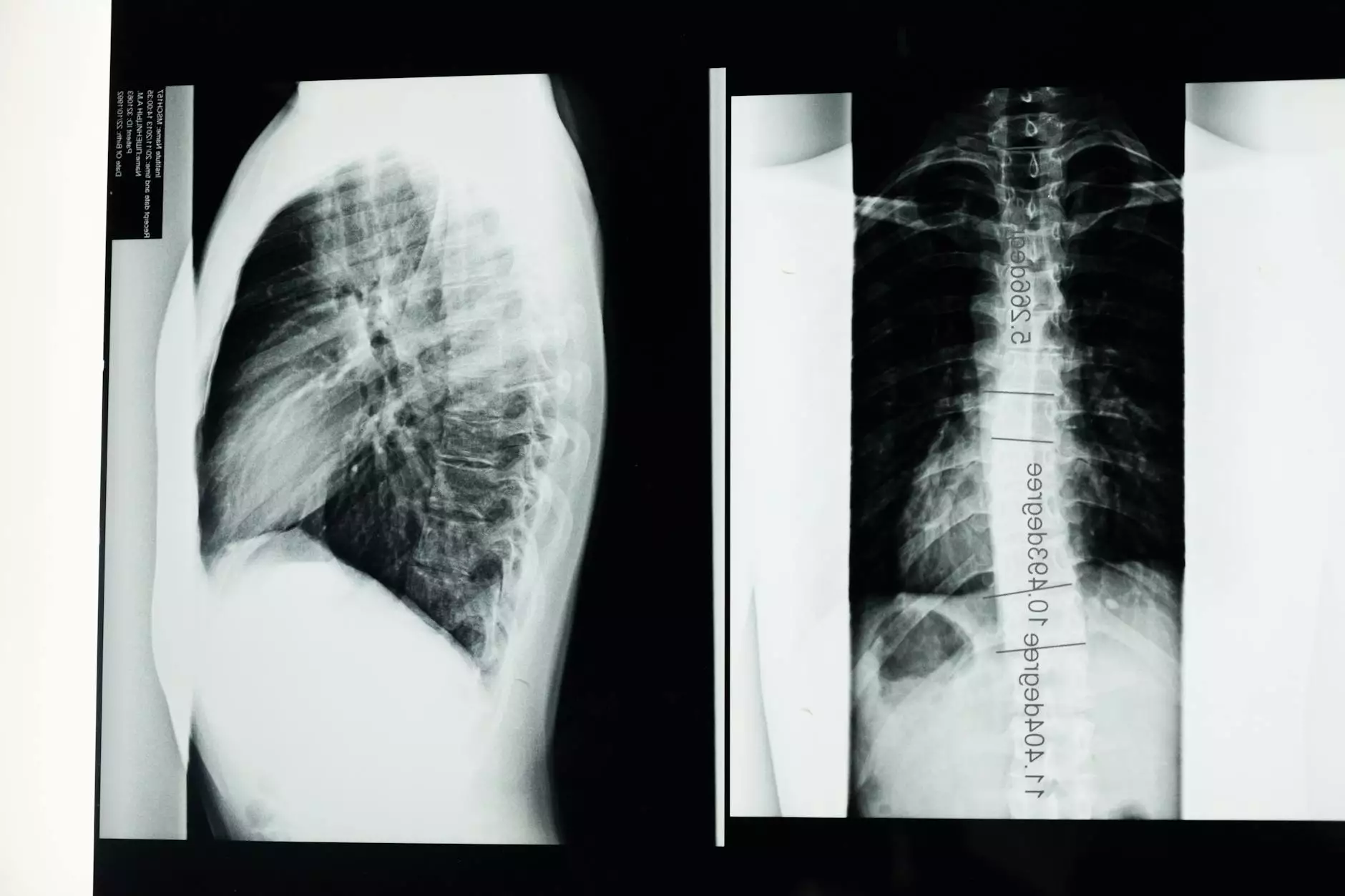
Diagnosis of Thoracic Hypomobility
Diagnosing thoracic hypomobility often involves a comprehensive evaluation by healthcare professionals, typically physical therapists or chiropractors. Common methods of assessment include:
- Physical Examination: The therapist will assess range of motion and check for tightness and tenderness in the thoracic region.
- Postural Assessment: Observing posture can help identify compensations and asymmetries in spinal alignment.
- Functional Movement Tests: Various activities may be analyzed to assess how thoracic mobility impacts functional movements.
Treatment Options for Thoracic Hypomobility
Effective management of thoracic hypomobility usually includes a combination of therapeutic approaches aimed at improving mobility, alleviating pain, and restoring a proper range of motion.
1. Physical Therapy
Physical therapy plays a crucial role in treating thoracic hypomobility. A licensed therapist will create personalized exercise regimens that may consist of:
- Stretching Exercises: Targeted stretching of the chest and shoulder muscles can enhance thoracic mobility.
- Strengthening Exercises: Focusing on strengthening the upper back muscles can help support better posture.
- Manual Therapy: Hands-on techniques applying pressure and movement can effectively increase mobility.
2. Chiropractic Care
Chiropractors specialize in spinal alignment and often utilize adjustments to restore proper motion and alleviate pain in the thoracic region. Regular adjustments can help maintain mobility, promote better posture, and enhance overall spinal function.
3. Ergonomic Adjustments
Making changes in daily activities, particularly in workplace ergonomics, can vastly improve thoracic mobility. Recommendations may include:
- Optimal Desk Setup: Ensuring the computer screen is at eye level to prevent forward head posture.
- Frequent Breaks: Taking short breaks to move and stretch can prevent stiffness from prolonged sitting.
- Smart Sitting: Using chairs that support the natural curve of the spine can encourage better posture.
4. Breathing Exercises
Incorporating breathing exercises into a daily routine can improve lung capacity and enhance thoracic mobility. Techniques such as diaphragmatic breathing, where the diaphragm is engaged during inhalation, can promote deeper and more effective breaths.
Self-Management Techniques for Thoracic Hypomobility
In addition to professional interventions, individuals can adopt self-management strategies to help reduce symptoms and enhance mobility:
1. Regular Physical Activity
Engaging in regular exercise can promote overall spinal health. Activities like swimming, yoga, and Pilates can be particularly beneficial for enhancing thoracic mobility while providing low-impact workout options.
2. Foam Rolling
Using a foam roller on the upper back can help release tension in the thoracic spine and surrounding muscles, promoting better mobility.
3. Mindfulness and Relaxation Techniques
Stress can exacerbate muscle tightness in the thoracic region. Implementing mindfulness practices such as meditation or yoga can relieve tension and improve overall well-being.
Conclusion
Thoracic hypomobility is a complex condition that can have significant implications for an individual's health and quality of life. By understanding its causes, recognizing the symptoms, and exploring available treatment options, patients can take proactive steps to manage and improve their condition. Ongoing education and collaboration with healthcare providers, such as those at IAOM-US, are vital for successfully navigating the challenges of thoracic hypomobility.
Ultimately, awareness and early intervention are key to preventing the long-term effects associated with thoracic hypomobility. By embracing a multifaceted approach that includes physical therapy, chiropractic care, ergonomic adjustments, and self-management techniques, individuals can regain mobility and enhance their overall quality of life. Remember, investing time in your health today can lead to a more functional and fulfilling tomorrow.









